Tag Archive for: UCLA Life Sciences

Kindness is contagious and these videos can help kids catch the altruism bug
UCLA researchers create video playlist for YouTube Kids’ anti-bullying…

Mentorship enhances mental health research focused on the underserved
Psychology professor Lauren Ng and doctoral student Yesenia Aguilar…
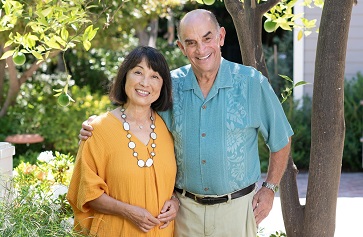
UCLA receives $1.5 million to further waterworks project at Mildred E. Mathias Botanical Garden
The gift from Charlie and Peggy Norris will help bring sustainable…

Patricia Greenfield honored for child development research
Patricia Greenfield, a UCLA distinguished professor of psychology,…

Camille Gaynus: Marine Scientist on a Mission
By Bekah Wright
Together, we can heal the oceans.
This…

Studying Maternal Stress
By Stuart Wolpert
Through their research with…

Neuroscientist Adriana Galván named 2021 Gold Shield Faculty Prize winner
Adriana Galván, dean of undergraduate education at UCLA,…

UCLA College to host virtual commencement celebration June 11
Civic leader, social justice advocate and UCLA alumnus D’Artagnan…

Migratory songbirds’ travels disrupted by earlier springs
Spring has arrived in North America. Leaves have sprouted,…

Five UCLA College professors elected to American Academy of Arts and Sciences
Eight faculty members, five of whom are from the UCLA College…

