Tag Archive for: UCLA Life Sciences
 https://www.college.ucla.edu/wp-content/uploads/2023/07/Bird_363.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-07-06 08:33:572023-07-06 08:33:57Birds raise fewer young when spring arrives earlier in a warming world
https://www.college.ucla.edu/wp-content/uploads/2023/07/Bird_363.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-07-06 08:33:572023-07-06 08:33:57Birds raise fewer young when spring arrives earlier in a warming world https://www.college.ucla.edu/wp-content/uploads/2023/06/Leopard_363.jpg
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-28 08:43:392023-06-28 08:43:39What’s living beneath the waves in Southern California?
https://www.college.ucla.edu/wp-content/uploads/2023/06/Leopard_363.jpg
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-28 08:43:392023-06-28 08:43:39What’s living beneath the waves in Southern California? https://www.college.ucla.edu/wp-content/uploads/2023/06/363AG.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-27 10:28:322023-06-27 10:28:32Andrew Goldstein receives grant from Department of Defense
https://www.college.ucla.edu/wp-content/uploads/2023/06/363AG.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-27 10:28:322023-06-27 10:28:32Andrew Goldstein receives grant from Department of Defense https://www.college.ucla.edu/wp-content/uploads/2023/06/ThienNguyen_363.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-15 14:16:072023-06-15 14:16:07First-gen transfer student takes aim at liver cancer
https://www.college.ucla.edu/wp-content/uploads/2023/06/ThienNguyen_363.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-15 14:16:072023-06-15 14:16:07First-gen transfer student takes aim at liver cancer
Once, twice, three times a Bruin
Graduating senior siblings Umiemah, Qasim and Humzah Farrukh…
 https://www.college.ucla.edu/wp-content/uploads/2023/06/CW_Commencement-2023-Web-Banner-1139x512-1-1.png
898
2000
Lucy Berbeo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Lucy Berbeo2023-06-15 08:15:122023-06-16 14:54:28UCLA College Class of 2023: Student Stories
https://www.college.ucla.edu/wp-content/uploads/2023/06/CW_Commencement-2023-Web-Banner-1139x512-1-1.png
898
2000
Lucy Berbeo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Lucy Berbeo2023-06-15 08:15:122023-06-16 14:54:28UCLA College Class of 2023: Student Stories https://www.college.ucla.edu/wp-content/uploads/2023/06/Grads_363.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-14 11:44:092023-08-10 13:57:55Congratulations, UCLA College Class of 2023!
https://www.college.ucla.edu/wp-content/uploads/2023/06/Grads_363.png
241
363
Alvaro Castillo
https://www.college.ucla.edu/wp-content/uploads/2019/07/Uxd_Blk_College-e1557344896161.png
Alvaro Castillo2023-06-14 11:44:092023-08-10 13:57:55Congratulations, UCLA College Class of 2023!
Nene Usim is charting her future in medicine
This graduating senior has long been turning compassion into…

Student singers uplift and inspire at UCLA College commencement
From left to right, UCLA College 2023 Commencement singers…
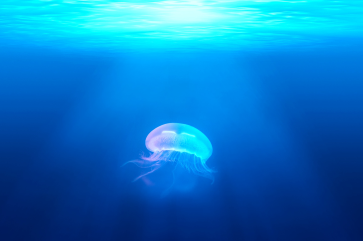
Disney mermaids aren’t the only wondrous creatures ‘under the sea’
On the eve of the ‘Little Mermaid’ premiere, a UCLA doctoral…

