Scientists identify a key gene in the transmission of deadly African sleeping sickness

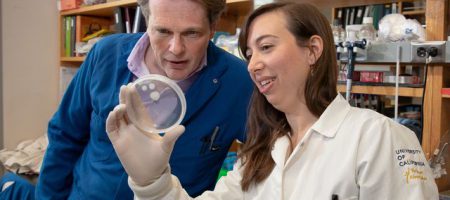
Research by UCLA professor Kent Hill and graduate student Stephanie DeMarco, as well as colleagues at the University of Bern, could lead to new approaches to treat African sleeping sickness.
Life scientists from UCLA and the University of Bern have identified a key gene in the transmission of African sleeping sickness — a severe disease transmitted by the bite of infected tsetse flies, which are common in sub-Saharan Africa.
The disease is fatal if untreated, as the parasite responsible moves from the bloodstream to the central nervous system. Tens of millions of people in 36 African countries are at risk. There is no vaccine, and conventional drug treatments, which include an arsenic derivative, are antiquated, not very effective and have severe side effects.
The research, published in the journal Nature Communications, could lead to new approaches to treat the disease. It also provides scientists with the first detailed understanding of how the parasite moves through the fly and what genes enable it to do so.
The tiny, single-celled parasite that causes African sleeping sickness in humans, and debilitating diseases in other mammals, is called Trypanosoma brucei, or T. brucei. To become infectious, the parasite must travel through tissues of the fly, from the midgut to the salivary gland — and then into the human or other animal, through a bite.
In the study, Stephanie DeMarco, a UCLA graduate student in molecular biology, and Sebastian Shaw, a graduate student at Switzerland’s University of Bern, worked with two sets of the T. brucei parasite. In one set, they made a mutation in one of the parasite’s genes, called phosphodiesterase-B1, or PDEB1.
Then, they infected 2,000 tsetse flies with some 20,000 parasites each — half of the flies received blood containing normal T. brucei parasites and the other half received blood with the mutated versions.
When tsetse flies drink infected blood, the parasites from the blood typically travel to the midgut and then into a tissue closer to the head, called the proventriculus, before moving on to the salivary glands.
But the researchers saw a striking difference in the proventriculus between the two sets of flies. Among the flies that received the normal parasites, those that had parasites in the gut also had parasites in the proventriculus; but among the 1,000 flies that received mutant T. brucei, only a single one that had parasites in the gut also had a parasite in the proventriculus.
“The normal parasites were able to get to the proventriculus just fine, but for the mutants, we saw only one lonely parasite swimming around,” DeMarco said. “That told us that phosphodiesterase-B1 is really important for the parasites to move from the fly midgut to the proventriculus.”
Shaw said, “When we saw the huge difference between the mutants and normal parasites, at first we couldn’t believe it.”
Kent Hill, a UCLA professor of microbiology, immunology and molecular genetics, and one of the study’s senior authors, said the findings also suggested that there must be a barrier preventing the mutants from getting from the midgut to the proventriculus.
To learn where that barrier is, the scientists made fluorescent parasites and fed the flies a fluorescent dye that stained different tissues in the fly different colors, enabling the researchers to track the parasites.
To go from the midgut to the proventriculus, the parasites have to cross the peritrophic matrix, a sheet-like structure produced by the proventriculus that protects the midgut.
“We found the normal parasites could get through the peritrophic matrix just fine, but the mutants were mostly stuck on one side of it,” DeMarco said.
That finding indicated that the peritrophic matrix was the barrier the scientists were looking for.
The research identifies for the first time the genes that enable the parasites to sense where they are and allow them to survive their journey in fly tissues; those mechanisms had not been understood well until now.
“We think the way the parasites perceive where they are may be similar in the tsetse flies and in mammals — including humans — as they go through barriers and tissues,” said co-senior author Isabel Roditi, a University of Bern professor. “If so, there could potentially be a new drug that might disrupt their ability to do that.”
The researchers also uncovered another clue to African sleeping sickness: In parasites with mutated PDEB1, there was a dramatic increase in the number of cyclic AMP molecules, signaling molecules that play an important role in the disease.
Normal parasites are social and coordinate their behavior, DeMarco said. But the research revealed that without PDEB1, the parasites have too much cyclic AMP in their cells and can’t communicate with one another.
“When Sebastian and Stephanie got rid of PDEB1, the parasites got flooded with cyclic AMP,” Hill said. “Then, when the signal came in telling the parasites, ‘You’re in the stomach and you need to move,’ they couldn’t hear the sound. That’s what we think the problem is for the mutant parasites.”
Hill said the new insights from the UCLA–Bern study could apply to other disease-causing parasites as well. For example, T. brucei parasites are related to parasites found in the U.S. and elsewhere that cause Chagas disease, in which parasites invade heart tissue, leading to inflammation and enlarged heart tissue, and in some cases, heart failure.
Hill’s research is funded by the National Institutes of Health’s National Institute of Allergy and Infectious Diseases and the National Institute of General Medical Sciences. Roditi’s research is funded by the Swiss National Science Foundation and the Howard Hughes Medical Institute.